Meet the virtual patients training real doctors
By Heather Kelly, CNN, Re-posted by Abdulgafar Abdulrauf Adio (www.econsforumnews.blogspot.com)
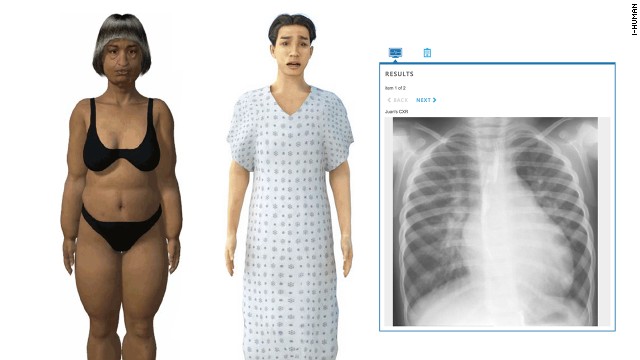 i-Human's interactive virtual patients are used by medical schools to train doctors how to diagnosis illnesses.
i-Human's interactive virtual patients are used by medical schools to train doctors how to diagnosis illnesses.
(CNN) -- Even before the examination begins, it's clear Ann Martinez isn't well.
 i-Human's interactive virtual patients are used by medical schools to train doctors how to diagnosis illnesses.
i-Human's interactive virtual patients are used by medical schools to train doctors how to diagnosis illnesses.(CNN) -- Even before the examination begins, it's clear Ann Martinez isn't well.
Her breathing is labored.
You can tell by the raspy sounds and jerky rise and fall of her chest.
Clad in her underwear, she waits quietly for the doctor, letting out the
occasional cough.
The physician starts by
going over her history, asking a few questions and taking her vitals.
Martinez, a smoker with a family history of heart disease, recently had
knee-replacement surgery. She confirms she's having trouble breathing
and complains of some chest pain. While checking her pulse, the doctor
notices that her heartbeat is faster than normal.
On their own, the
symptoms are too common to reach any immediate conclusion. It's possible
she has a simple chest cold, but the signs could indicate something
more dangerous, even fatal. More tests are needed.
There's no risk of
Martinez dying, however, because she isn't real. She is a naturalistic,
interactive virtual patient that lives on a computer screen. The
simulation is part of i-Human Patients, one of a new generation of computer programs used by medical schools to train students and other professionals.
Like a flight simulator
for doctors, i-Human presents cases as complicated, hands-on puzzles
that require real medical skills to figure out. There is minimal
guidance or hand-holding, leaving students to make hundreds of little
decisions and conduct tests as they would when diagnosing a real sick
person.
"A patient shows up in
your office, and that's it. That's real life. You need to start asking
questions," said Norm Wu, CEO of i-Human.
I-Human says its program is an evolution of the popular first-generation virtual patients like InTime's MedU,
which are still used in most medical schools. Those programs and
documents also ask medical students to make a diagnosis but typically
with text, multimedia prompts and multiple choice options.
Medical schools also rely
on a combination of actors and mannequins to help train doctors. Both
have their advantages; working with an actor is great for bedside manner
and interpersonal skills. But they can be expensive, and taking them
home to practice isn't really an option. With a cloud-based computer
program, a medical student can practice his or her diagnoses anywhere
there's Wi-Fi. Data can be collected to let professors know how students
are progressing, highlighting areas where they need improvement.
"If you're a medical
school professor, it's very easy to test for fact-based recall," Wu
said. "How do you tell if somebody has figured out how to appropriately
assess and diagnosis a patient with minimum error?"
Realistic high-tech
training programs like i-Human aren't just another helpful tool. They
have the potential to address a shortage of trained doctors and nurses.
The U.S. Department of Health and Human Services predicts a shortage of more than 20,000 primary care physicians by 2020, driven largely by the aging of baby boomers.
The issue is more severe
in developing countries like India, where there is an average of one
doctor per 1,700 people. In some Indian states the number is closer to 1
per 10,000, and hard-to-reach rural areas
are far worse. Over the next 16 years, India's government wants to
train 1.6 million new physicians. Technology could play a huge role in
the country, where doctors and brick-and-mortar med schools aren't
plentiful.
I-Human is working with
20 educators in India to localize the program, customizing patients and
illnesses for the target market. (It has added an option for more
conservative gowned avatars.)
More accessible
diagnostic training for medical schools could also have an impact on the
misdiagnosis rate. One out of every 20 outpatients is misdiagnosed in
the U.S., according to an April study by BMJ Quality and Safety Journal -- that's 12 million cases a year.
Craig and Anne Knoche
think that more realistic training could dramatically lower that number.
The pair of Silicon Valley veterans launched i-Human with Corey
Cerovsek in 2012 after creating standalone medical simulators for years.
Currently at use in 14
medical schools, the virtual patients are diagnosed as homework, group
projects and tests and as a teaching tool in front of a class. The
program has optional coaching tools like prompts, lessons and quizzes to
keep beginning students on the right track, a common issue when there
are thousands of possible questions to ask and hundreds of labs and
tests to order.
Practicing on an avatar,
no matter how realistic their gout or pneumonia, is obviously not the
same as treating a real human. But a team of graphic artists has worked
to make the avatars mimic real illness as much as possible. The team
designs five or six new "patients" a week.
Each virtual patient has
a name, a medical history, symptoms and an illness. They are a diverse
selection of 3-D illustrations, with realistically rendered bodies,
which makes it possible to see problems like jaundiced skin at a glance.
Audio and animations tip students off to key details, like the sound of
wheezing or the way a patient blinks.
Schools and other third
parties can build their own cases using i-Human and share them with
other customers, similar to selling apps in Apple's App Store. The cases
are peer-reviewed and subject to a review by i-Human's two full-time
staff physicians.
The virtual physical
exams simulates, as much as possible on a screen, the tactical skills
needed for things like measuring blood pressure and testing pupil
reactions. To hear Ann Martinez's heart, the student must know where
exactly to put the stethoscope.
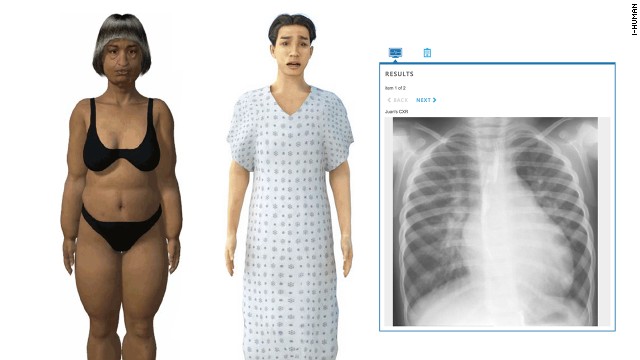
Eventually, if they're
on the right track, Martinez's doctor will order a battery of tests that
include a CT pulmonary angiogram. The result, a black and white image
of real arteries, shows a pulmonary embolism. Pulmonary embolisms are
frequently misdiagnosed and are the third most common cause of death in
hospitalized patients.
If the medical student orders the correct course of treatment, Martinez will live another day and train more future doctors.










0 comments:
Post a Comment